@maxdancona,
https://www.nytimes.com/2020/03/13/us/coronavirus-deaths-estimate.html
Worst-Case Estimates for U.S. Coronavirus Deaths
Projections based on C.D.C. scenarios show a potentially vast toll. But those numbers don’t account for interventions now underway.
The C.D.C. scenarios have not been publicly disclosed. Without an understanding of how experts view the threat, it remains unclear how far Americans will go in adopting socially disruptive steps that could help avert deaths.
The C.D.C. scenarios have not been publicly disclosed. Without an understanding of how experts view the threat, it remains unclear how far Americans will go in adopting socially disruptive steps that could help avert deaths.Credit...Erin Schaff/The New York Times
Sheri Fink
By Sheri Fink
Published March 13, 2020
Updated March 18, 2020
Officials at the U.S. Centers for Disease Control and Prevention and epidemic experts from universities around the world conferred last month about what might happen if the new coronavirus gained a foothold in the United States. How many people might die? How many would be infected and need hospitalization?
One of the agency’s top disease modelers, Matthew Biggerstaff, presented the group on the phone call with four possible scenarios — A, B, C and D — based on characteristics of the virus, including estimates of how transmissible it is and the severity of the illness it can cause. The assumptions, reviewed by The New York Times, were shared with about 50 expert teams to model how the virus could tear through the population — and what might stop it.
The C.D.C.’s scenarios were depicted in terms of percentages of the population. Translated into absolute numbers by independent experts using simple models of how viruses spread, the worst-case figures would be staggering if no actions were taken to slow transmission.
Between 160 million and 214 million people in the United States could be infected over the course of the epidemic, according to a projection that encompasses the range of the four scenarios. That could last months or even over a year, with infections concentrated in shorter periods, staggered across time in different communities, experts said. As many as 200,000 to 1.7 million people could die.
And, the calculations based on the C.D.C.’s scenarios suggested, 2.4 million to 21 million people in the United States could require hospitalization, potentially crushing the nation’s medical system, which has only about 925,000 staffed hospital beds. Fewer than a tenth of those are for people who are critically ill.
The assumptions fueling those scenarios are mitigated by the fact that cities, states, businesses and individuals are beginning to take steps to slow transmission, even if some are acting less aggressively than others. The C.D.C.-led effort is developing more sophisticated models showing how interventions might decrease the worst-case numbers, though their projections have not been made public.
“When people change their behavior," said Lauren Gardner, an associate professor at the Johns Hopkins Whiting School of Engineering who models epidemics, “those model parameters are no longer applicable,” so short-term forecasts are likely to be more accurate. “There is a lot of room for improvement if we act appropriately.”
Those actions include testing for the virus, tracing contacts, and reducing human interactions by stopping mass gatherings, working from home and curbing travel. In just the last two days, multiple schools and colleges closed, sports events were halted or delayed, Broadway theaters went dark, companies barred employees from going to the office and more people said they were following hygiene recommendations.
The Times obtained screenshots of the C.D.C. presentation, which has not been released publicly, from someone not involved in the meetings. The Times then verified the data with several scientists who did participate. The scenarios were marked valid until Feb. 28, but remain “roughly the same,” according to Ira Longini, co-director of the Center for Statistics and Quantitative Infectious Diseases at the University of Florida. He has joined in meetings of the group.
The C.D.C. declined interview requests about the modeling effort and referred a request for comment to the White House Coronavirus Task Force. Devin O’Malley, a spokesman for the task force, said that senior health officials had not presented the findings to the group, led by Vice President Mike Pence, and that nobody in Mr. Pence’s office “has seen or been briefed on these models.”
The assumptions in the C.D.C.’s four scenarios, and the new numerical projections, fall in the range of others developed by independent experts.
Dr. Longini said the scenarios he helped the C.D.C. refine had not been publicly disclosed because there remained uncertainty about certain key aspects, including how much transmission could occur from people who showed no symptoms or had only mild ones.
“We’re being very, very careful to make sure we have scientifically valid modeling that’s drawing properly on the epidemic and what’s known about the virus,” he said, warning that simple calculations could be misleading or even dangerous. “You can’t win. If you overdo it, you panic everybody. If you underdo it, they get complacent. You have to be careful.”
But without an understanding of how the nation’s top experts believe the virus could ravage the country, and what measures could slow it, it remains unclear how far Americans will go in adopting — or accepting — socially disruptive steps that could also avert deaths. And how quickly they will act.
Studies of previous epidemics have shown that the longer officials waited to encourage people to distance and protect themselves, the less useful those measures were in saving lives and preventing infections.
ImageAn isolate from the first U.S. case of Covid-19, the illness caused by coronavirus.
“A fire on your stove you could put out with a fire extinguisher, but if your kitchen is ablaze, that fire extinguisher probably won’t work,” said Dr. Carter Mecher, a senior medical adviser for public health at the Department of Veterans Affairs and a former director of medical preparedness policy at the White House during the Obama and Bush administrations. “Communities that pull the fire extinguisher early are much more effective.”
Dr. Biggerstaff presented his scenarios in a meeting held weekly to model the pandemic’s effects in the United States, Dr. Longini said. Its participants had been at work for several months before the emergence of the virus, modeling a potential influenza pandemic. “We just kind of retooled, re-shifted,” said Dr. Longini. “The priority’s now coronavirus.”
Latest Updates: Coronavirus Outbreak in the U.S.
The four scenarios have different parameters, which is why the projections range so widely. They variously assume that each person with the coronavirus would infect either two or three people; that the hospitalization rate would be either 3 percent or 12; and that either 1 percent or a quarter of a percent of people experiencing symptoms would die. Those assumptions are based on what is known so far about how the virus has behaved in other contexts, including in China.
Other weekly C.D.C. modeling meetings center on how the virus is spreading internationally, the impact of community actions such as closing schools, and estimating the supply of respirators, oxygen and other resources that could be needed by the nation’s health system, participants said.
In the absence of public projections from the C.D.C., outside experts have stepped in to fill the void, especially in health care. Hospital leaders have called for more guidance from the federal government as to what might lie in store in the coming weeks.
Even severe flu seasons stress the nation’s hospitals to the point of setting up tents in parking lots and keeping people for days in emergency rooms. Coronavirus is likely to cause five to 10 times that burden of disease, said Dr. James Lawler, an infectious diseases specialist and public health expert at the University of Nebraska Medical Center. Hospitals “need to start working now,” he said, “to get prepared to take care of a heck of a lot of people.”
Dr. Lawler recently presented his own “best guess” projections to American hospital and health system executives at a private webinar convened by the American Hospital Association. He estimated that some 96 million people in the United States would be infected. Five out of every hundred would need hospitalization, which would mean close to five million hospital admissions, nearly two million of those patients requiring intensive care and about half of those needing the support of ventilators.
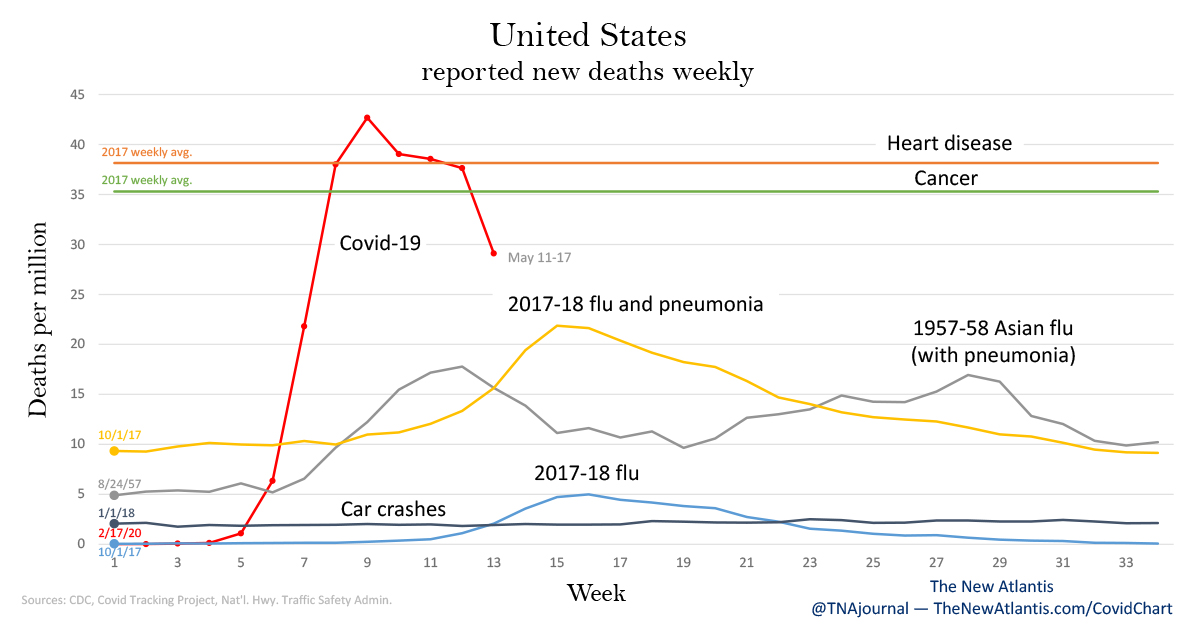
Dr. Lawler’s calculations suggested 480,000 deaths, which he said was conservative. By contrast, about 20,000 to 50,000 people have died from flu-related illnesses this season, according to the C.D.C. Unlike with seasonal influenza, the entire population is thought to be susceptible to the new coronavirus.
Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, speaking at a congressional hearing on Thursday, said predictions based on models should be treated with caution. “All models are as good as the assumptions that you put into the model,” he said, responding to a question from Representative Rashida Tlaib about an estimate from the attending physician of Congress that the United States could have 70 million to 150 million coronavirus cases.
What will determine the ultimate number, he said, “will be how you respond to it with containment and mitigation.”
Clues From 1918
Independent experts said these projections were critically important to act on, and act on quickly. If new infections can be spread out over time rather than peaking all at once, there will be less burden on hospitals and a lower ultimate death count. Slowing the spread will paradoxically make the outbreak last longer, but will cause it to be much milder, the modelers said.
A preliminary study released on Wednesday by the Institute for Disease Modeling projected that in the Seattle area, enhancing social distancing — limiting contact with groups of people — by 75 percent could reduce deaths caused by infections acquired in the next month from 400 to 30 in the region.
A recent paper, cited by Dr. Fauci at a news briefing on Tuesday, concludes that the rapid and aggressive quarantine and social distancing measures applied by China in cities outside of the outbreak’s epicenter achieved success. “Most countries only attempt social distancing and hygiene interventions when widespread transmission is apparent. This gives the virus many weeks to spread,” the paper said, with the average number of people each new patient infects higher than if the measures were in place much earlier, even before the virus is detected in the community.
“By the time you have a death in the community, you have a lot of cases already,” said Dr. Mecher. “It’s giving you insight into where the epidemic was, not where it is, when you have something fast moving.” He added: “Think starlight. That light isn’t from now, it’s from however long it took to get here.”
He said a single targeted step — a school closing, or a limit on mass gatherings — cannot stop an outbreak on its own. But as with Swiss cheese, layering them together can be effective.
This conclusion is backed up by history.
The most lethal pandemic to hit the United States was the 1918 Spanish flu, which was responsible for about 675,000 American deaths, according to estimates cited by the C.D.C.
The Institute for Disease Modeling calculated that the new coronavirus is roughly equally transmissible as the 1918 flu, and just slightly less clinically severe, and it is higher in both transmissibility and severity compared with all other flu viruses in the past century.
Dr. Mecher and other researchers studied deaths during that pandemic a century ago, comparing the experiences of various cities, including what were then America’s third- and fourth-largest, Philadelphia and St Louis. In October of that year Dr. Rupert Blue, America’s surgeon general, urged local authorities to “close all public gathering places if their community is threatened with the epidemic,” such as schools, churches, and theaters. “There is no way to put a nationwide closing order into effect,” he wrote, “as this is a matter which is up to the individual communities.”
The mayor of St. Louis quickly took that advice, closing for several weeks “theaters, moving picture shows, schools, pool and billiard halls, Sunday schools, cabarets, lodges, societies, public funerals, open air meetings, dance halls and conventions until further notice.” The death rate rose, but stayed relatively flat over that autumn.
By contrast, Philadelphia took none of those measures; the epidemic there had started before Dr. Blue’s warning. Its death rate skyrocketed.
The speed and deadliness of the pandemic humbled doctors then much as the coronavirus pandemic is doing now. Some commented on the difficulty of getting healthy people to take personal precautions to help protect others at greater risk.
Modern societies have tools that did not exist then: advanced hospitals, the possibility of producing a vaccine in roughly a year, the production of diagnostics. But other signs are more worrying.
The world population is about triple the size it was the year before the 1918 flu, with 10 times as many people over 65 and 30 times as many over 85. These groups have proven especially likely to become critically ill and die in the current coronavirus pandemic. In Italy, hospitals are so overwhelmed that ventilators are being rationed.
“It’s so important that we protect them,” said Dr. Gabriel Leung, a professor in population health at Hong Kong University. In work accepted for publication in the journal Nature Medicine, he estimated that 1.5 percent of symptomatic people with the virus died. He and others who have devoted their careers to modeling said that looking at the experiences of other countries already battling the coronavirus was all it took to know what needed to be done in the United States.
“All U.S. cities and states have the natural experiment of the cities that have preceded us, namely the superb response of Singapore and Hong Kong,” said Dr. Michael Callahan, an infectious disease specialist at Harvard. Those countries implemented school closures, eliminated mass gatherings, required work from home, and rigorously decontaminated their public transportation and infrastructure. They also conducted widespread testing.
They were able to “reduce an explosive epidemic to a steady state one,” Dr. Callahan said.
As in the case of an approaching hurricane, Dr. Mecher said, “You’ve got to take potentially very disruptive actions when the sun is shining and the breeze is mild.”